Exceptional Senior Living in East Bay, CA for Comfort & Care
When searching for Westmont of Pinole, families often want clarity, comfort, and confidence in choosing the right home for aging loved ones. Today’s older adults deserve environments that strengthen independence, nurture connection, and offer personalized care. That’s why finding the right senior living community in the East Bay, CA, can make all the difference in achieving safety, comfort, and joy.
At Westmont of Pinole, residents experience thoughtful support, wellness-focused programs, and engagement opportunities that uplift daily life. Whether you’re exploring assisted living or memory care, this community stands out among the best senior living in East Bay, CA, for its compassion-driven approach and vibrant lifestyle offerings.
For more information, visit their website at Westmont of Pinole.
Exploring Assisted Living Options
When considering assisted living, how do you ensure the community you choose aligns with your loved one’s goals and well-being? Begin by understanding the benefits and lifestyle enhancements available. Westmont of Pinole, known for its commitment to senior living in East Bay, CA, provides care plans and supportive services tailored to individual needs.
Schedule tours, meet the staff and residents, and take time to observe the environment. These interactions offer clarity as you compare amenities, care plans, and activity calendars. You’re not simply selecting a place to live—you’re choosing a home that encourages independence, comfort, and engagement.
Customized care plans help ensure that each individual receives the personalized attention they deserve, making this one of the best senior living communities in East Bay, CA, for families seeking high-quality care.
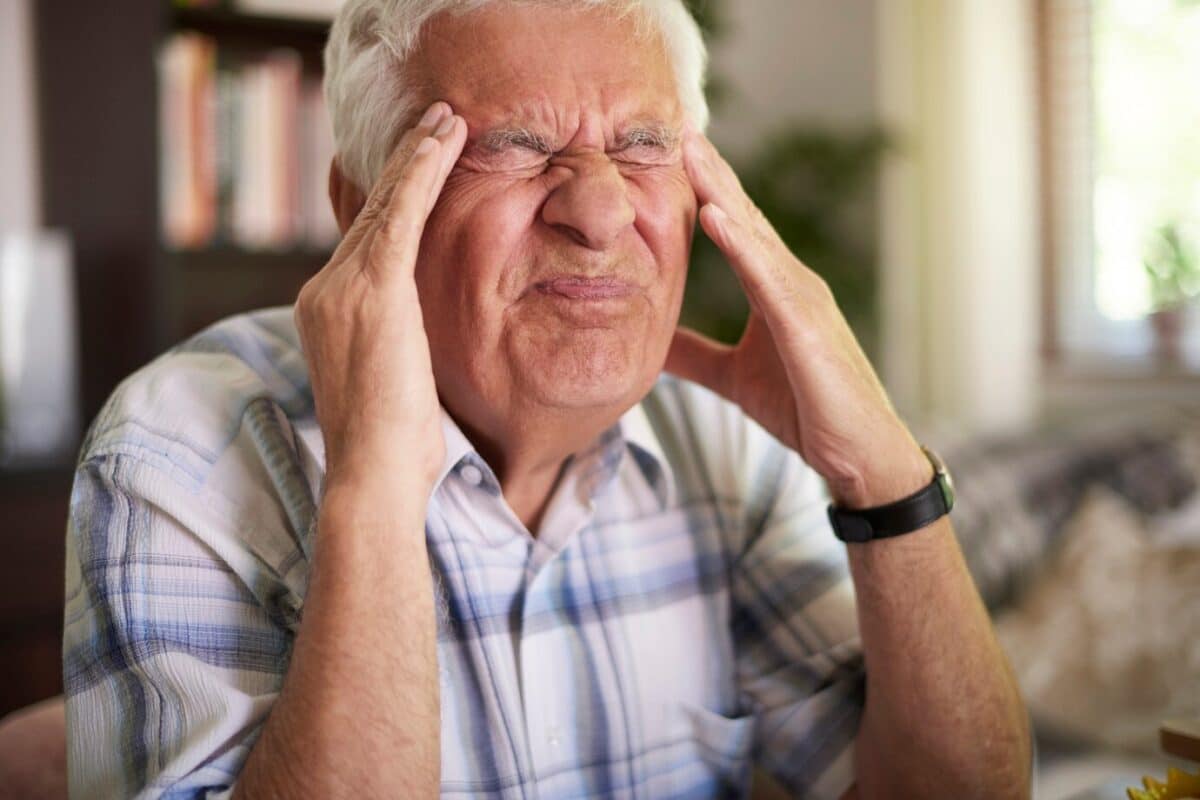
Understanding Memory Care Services
Memory care requires a specialized environment rooted in trust, routine, and compassionate support. Westmont of Pinole provides structured care tailored to residents living with cognitive changes, reinforcing its reputation as a Bay Area luxury retirement community that emphasizes both safety and comfort.
You’ll find personalized care plans, secure spaces, and enriching activities built around memory support. These programs strengthen familiarity, reduce stress, and help residents feel valued and connected every day.
Memory care facilities also provide engaging activities tailored to cognitive function, elevating the quality of life for each resident.
Personalized Care Plans
A strong memory care program begins with individualized assessments, allowing caregivers to build tailored care strategies. This customized approach—central to senior living in East Bay, CA communities—ensures residents receive focused support designed for their unique journey.
| Element | Description | Purpose |
| Personalized Assessments | Evaluations to understand needs | Identify necessary care |
| Tailored Interventions | Individualized strategies | Enhance daily life |
| Regular Updates | Ongoing plan adjustments | Meet evolving needs |
| Family Involvement | Collaboration with loved ones | Strengthen support |
| Staff Training | Education on memory care | Maintain high-quality care |
Learn more about quality memory care and why personalization remains key to dignity and comfort.
Safety and Security Measures
Safety is an essential part of memory care. Westmont of Pinole embraces best practices such as secure entrances, highly trained staff, and emergency preparedness protocols. These safeguards ensure residents feel supported, reducing stress for both families and the individual.
Evaluating senior communities also means reviewing their safety standards. Tools like quality in assisted living help families ensure the environment aligns with industry best practices.
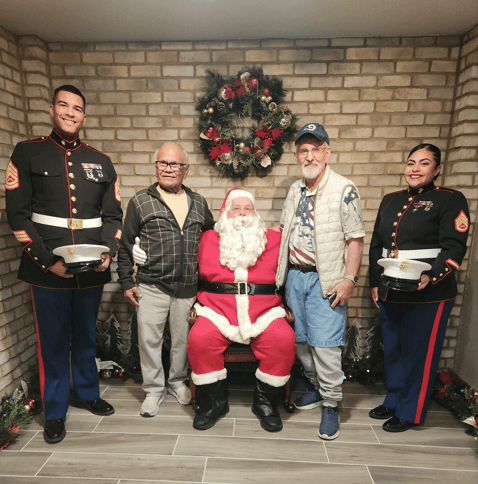
Engaging Activities and Programs
Daily activities stimulate the mind, foster connection, and build a sense of accomplishment. Creative workshops, social outings, and movement-focused programs help residents experience joy, purpose, and connection.
The use of technology-assisted therapies enhances cognitive and emotional well-being, a growing standard in Bay Area luxury retirement communities.

Amenities and Support for Residents
At 1440 By The Bay, amenities are thoughtfully designed to uplift the lifestyle of every resident. Though distinct from Westmont of Pinole, its model illustrates how compassionate environments enhance senior living in East Bay, CA. From activities to dining, each feature serves a purpose—community, comfort, and engagement.
Comprehensive Wellness Services
Health and wellness services play a central role in senior well-being. At 1440 By The Bay, comprehensive care includes:
- Onsite Wellness Services
- Transportation Support
- Move-In Coordination
These programs mirror the importance of wellness in the best senior living in East Bay, CA, where residents thrive with support tailored to changing needs.
Engaging Community Activities
A lively social environment helps seniors maintain emotional health. Activities such as book clubs, fitness classes, art workshops, and community events foster meaningful connections and offer growth opportunities.
Culinary Dining Experiences
Dining isn’t just nourishment—it’s community. From chef-prepared meals to seasonal menus, culinary programs prioritize flavor, nutrition, and social connection, a hallmark of luxury retirement communities in Bay Area living.
Importance of Wellness and Health Services
Wellness initiatives support long-term independence and vitality. Regular screenings, mental health support, and fitness programs help residents remain active and engaged. These wellness-centered approaches reflect what families expect from the best senior living in East Bay, CA, and bolster overall quality of life.
Engaging Community Life and Activities
Connection is at the heart of healthy aging. Through diverse social opportunities—workshops, events, clubs—residents can remain active, vibrant, and fulfilled. Community life strengthens emotional well-being and helps shape a meaningful experience in a supportive environment.
Dining Experiences for Residents
Thoughtfully curated menus, nutrition-forward meals, and personalized dining support create a warm setting for residents to connect over shared tables. With flexible dining schedules and dedicated culinary teams, residents enjoy comfort, flavor, and companionship.
Choosing the Right Residence for Comfort
Choosing the right residence means looking at amenities, care services, location, and community culture. Consider features that enhance daily life and support independence. A nurturing environment—such as the one found at Westmont of Pinole—ensures residents feel valued, supported, and at home.
Ready to Experience the Best Senior Living in East Bay, CA?
Choosing the right community can transform your loved one’s life—bringing comfort, joy, independence, and connection. Westmont of Pinole stands proudly among the best senior living in East Bay, CA, and continues to set the standard for compassionate support and vibrant lifestyle programming.
Explore what makes this one of the premier luxury retirement communities in Bay Area living. Call us today at 510-758-1122 or schedule your visit at Schedule a Tour.
Your family deserves confidence. Your loved one deserves comfort. Westmont of Pinole delivers both.
Frequently Asked Questions
What is the average cost of senior living in California?
The average cost of senior living in California varies by location and level of care, but most seniors can expect to pay between $4,500 and $7,000 per month. Assisted living generally falls around the mid-range, while memory care communities typically cost more due to specialized support. Luxury communities in metropolitan areas like the Bay Area or Los Angeles often have higher monthly rates. Costs may also include amenities, meals, and personal care services, depending on the community.
What is the cheapest way for a senior to live?
The most affordable living option for seniors often includes aging in place with limited in-home support, shared housing, or moving to subsidized senior housing programs. Seniors may also explore government assistance options such as HUD housing or state-based financial aid. Some choose to live with family members to reduce expenses and receive informal support. Budget-friendly communities exist, but availability and eligibility can vary widely.
Where is the best place for seniors to live in California?
The best place for seniors to live in California depends on their lifestyle, care needs, and budget. Areas like San Diego, Sacramento, and the Central Coast are often praised for mild weather, strong healthcare systems, and senior-friendly communities. The Bay Area offers excellent amenities and cultural opportunities, though it tends to cost more. Many seniors also consider smaller suburban cities for a quieter environment and lower expenses.
Is East Bay cheaper?
The East Bay is generally more affordable than other parts of the Bay Area, particularly San Francisco and Silicon Valley. While prices are still higher than in many other U.S. regions, seniors often find more budget-friendly housing options here. Cities like Pinole, Richmond, and Oakland offer diverse senior living choices at varying price points. However, costs still depend on community type, amenities, and level of care needed.