Depression and Memory Loss: What You Need to Know Now
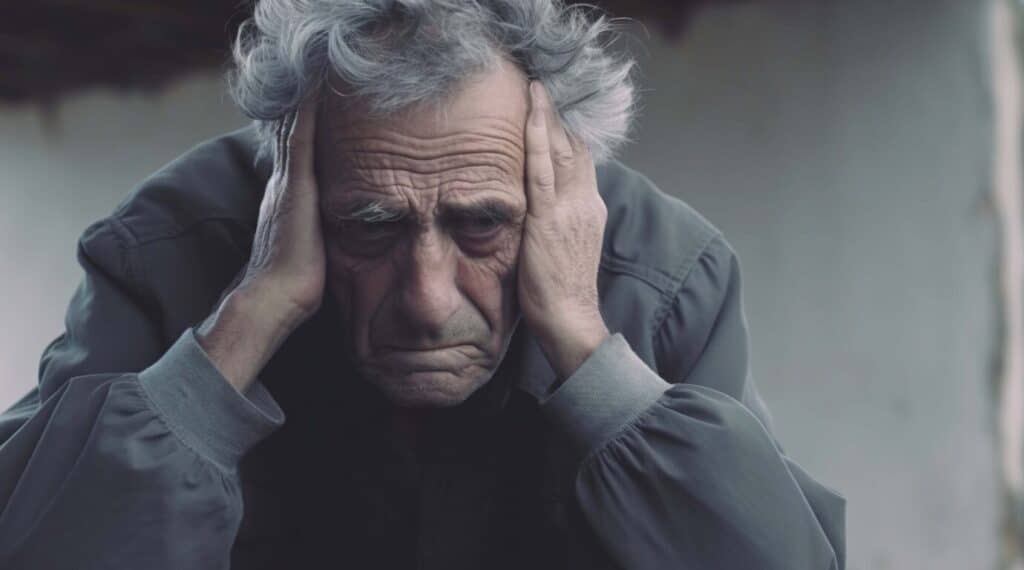
Experiencing depression and memory loss together can feel like you’re trapped in a fog, unable to think clearly or remember simple things. Many people don’t realize that depression doesn’t just affect mood—it can also disrupt your memory and thinking skills. If you’ve ever asked, Does depression affect memory?—The answer is yes, and research continues to uncover how deep that connection runs. Symptoms like forgetfulness, indecision, and confusion can all be rooted in emotional health. These cognitive changes often mimic early dementia symptoms, adding to the distress. Fortunately, understanding the link between mood and memory can empower individuals to seek help. Regaining mental clarity and confidence through treatment and community support is possible. At Westmont of Morgan Hill, we offer resources that provide real solutions. If you’re concerned about memory problems linked to mood, you’re not alone—and help is closer than you think.
How Does Depression Affect Memory?
If you’ve ever wondered, can depression cause memory loss? Science says yes. Depression can slow down your brain’s ability to store and recall information. You might find it hard to focus on tasks or forget details you just learned. Studies suggest chronic sadness alters brain function, especially in working memory and learning. When constantly battling negative thoughts, your brain has less energy to focus on remembering things. So, if you’re struggling with attention or forgetfulness, it’s not just in your head—it’s your brain signaling that it needs care. This is why early recognition of depression and memory loss is key to recovery. Therapy, medication, or lifestyle changes can start making a difference sooner than you think.
Explore how depression impacts memory and discover tools that support mental clarity.
Recognizing the Early Signs of Cognitive Decline
Noticing unusual memory lapses can be unsettling. You may find yourself repeating questions or forgetting everyday routines. These small moments add up and become more disruptive over time. Depression often heightens these issues. People may misplace items, forget conversations, or struggle with word-finding. These aren’t just side effects but symptoms of deeper problems affecting brain health. And while dementia might be a concern, often these symptoms stem from treatable causes. Recognizing the link between depression and memory loss early allows for faster depression memory loss treatment that can reduce cognitive fog and improve functioning. At Westmont of Morgan Hill, we support residents through holistic memory care programs that address emotional and mental needs.
Learn how to spot memory challenges early and when to seek guidance.
What Happens During Diagnosis
Getting help starts with understanding what’s going on. The diagnostic process usually begins with a physical exam to rule out other causes, like thyroid problems or vitamin deficiencies, that may mimic depression symptoms. Once medical conditions are ruled out, providers move on to mental health assessments. These often include cognitive testing to pinpoint how memory and thinking are affected. During these evaluations, professionals can determine whether your memory issues are connected to mood disorders. If you’ve been wondering, does depression affect memory?, assessments can give you the clarity and direction you need. The correct diagnosis leads to the right care, which makes all the difference.
Visit specialized geriatric care resources to learn more about the evaluation process.
The Power of Treatment and Recovery
Hope is accurate, and recovery is possible. With the right combination of treatment, many people experience remarkable improvements in both mood and memory. Depression memory loss treatment typically involves antidepressants, which not only lift mood but also improve attention and recall. Therapy, especially Cognitive Behavioral Therapy (CBT), is another powerful tool. It helps retrain the brain to respond differently to stress, improving mental outlook and cognitive sharpness. Lifestyle also plays a role—adequate sleep, exercise, and a nutritious diet all support brain function. Suppose you’ve been asking whether depression and memory loss recovery is possible. In that case, the answer is yes—with the proper support and persistence, many people return to complete mental clarity and emotional stability.
Recovery starts with one step—reach out to professionals who can guide you.
Discover the level of care you or your family member requires.What Level of Care Do You Need?
Community Support is Essential for Healing
You’re never alone in this journey. Many individuals and families face similar challenges, and connecting with others can reduce isolation and fear. Community resources like support groups, mental wellness programs, and caregiver networks offer a lifeline. These services don’t just provide information—they offer connection, understanding, and encouragement. Joining a support group allows individuals to share their experiences, learn from others, and develop healthier coping strategies. It’s a step toward healing that reinforces your emotional strength. At Westmont of Morgan Hill, we encourage families and individuals to explore these opportunities. The bond of shared experience can do more for recovery than you might imagine.
Tap into community support networks near you and take your next step toward healing.

Creating a Plan for Long-Term Wellness
To indeed manage the impact of depression and memory loss, a long-term strategy is vital. This includes consistent medical care, regular mental health check-ins, and lifestyle adjustments prioritizing cognitive health. Whether improving sleep habits or reducing stress through mindfulness, small changes can lead to significant improvements. Remember: even if symptoms overwhelm, the brain can change and heal. Regular engagement in stimulating activities—like puzzles, reading, or music—helps keep your mind active and sharp. Involving loved ones in your care plan can also ensure you’re surrounded by people who understand and support your needs.
If you’ve been asking, can depression cause memory loss?, it’s time to act on the answer and take proactive steps.
You’re Not Alone—We’re Here to Help
Understanding the complex relationship between depression and memory loss is the first step toward healing. The next is reaching out. Whether you’re facing mild memory lapses or navigating more profound emotional struggles, help is within reach. At Westmont of Morgan Hill, our compassionate team is ready to support you with resources tailored to your needs—from professional counseling to memory care programs that enhance everyday life. Don’t wait for the fog to lift on its own. Take the first step and reclaim your clarity.
Call Westmont of Morgan Hill today at 408-779-8490 to get the support you deserve.

Frequently Asked Questions
Is memory loss a side effect of depression?
Yes, memory loss can be a side effect of depression. Many people with depression experience difficulty concentrating, remembering details, or making decisions. These cognitive symptoms are often called “brain fog” and can affect daily functioning. It’s essential to recognize that this is a common and treatable aspect of depression.
Can memory loss from depression be reversed?
Memory issues caused by depression are often reversible with proper treatment. As mood improves through therapy, medication, or lifestyle changes, cognitive functions like memory and focus typically return to normal. However, recovery time can vary from person to person. Early intervention often leads to better outcomes.
How to pull yourself out of a depressive episode?
Pulling yourself out of a depressive episode often involves a combination of small, manageable steps. These can include reaching out for support, establishing a routine, practicing self-care, and staying physically active. Professional help, such as therapy or medication, can also be crucial. Be patient with yourself—healing takes time and persistence.
What are the symptoms of a depressive episode?
A depressive episode is marked by persistent sadness, loss of interest or pleasure in activities, fatigue, and changes in sleep or appetite. Other symptoms may include feelings of worthlessness, difficulty concentrating, and thoughts of hopelessness or suicide. These symptoms usually last at least two weeks and can vary in severity. Seeking help if you’re experiencing any of these signs is essential.








