Understanding the Progression of Senior Alzheimer’s Disease
Caring for someone with senior Alzheimer’s disease can feel overwhelming, but understanding the condition and knowing what care options are available can make all the difference. From recognizing the early symptoms of Alzheimer’s disease to exploring specialized care like memory support, every decision you make helps improve your loved one’s quality of life.
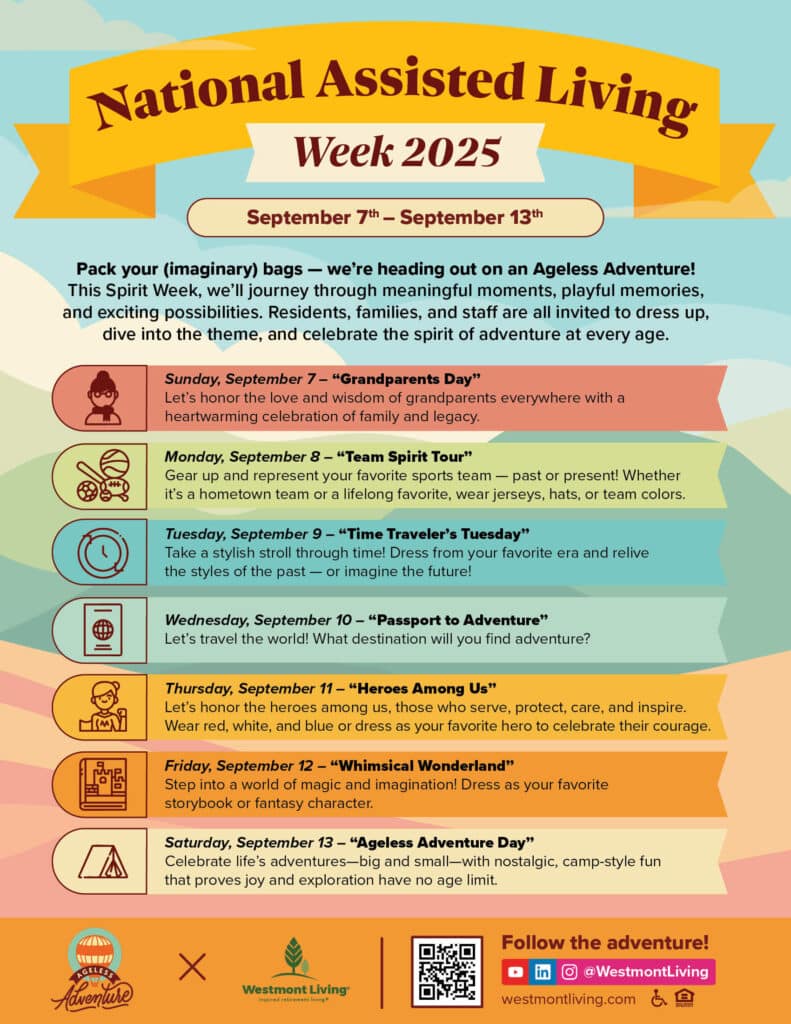
In this guide, we’ll walk you through how memory care adapts to the progression of Alzheimer’s. You’ll learn about different types of Alzheimer’s disease, current innovations in Alzheimer’s disease treatment, and how support from places like Westmont of La Mesa can help families navigate this difficult journey with greater ease.
Understanding What is Alzheimer’s Disease
Defining the Disease
What is Alzheimer’s disease? It’s a progressive brain disorder that slowly destroys memory, thinking skills, and eventually the ability to carry out the simplest tasks. Most commonly affecting seniors, it’s the most prevalent form of dementia, accounting for 60–80% of dementia cases.
Early intervention is crucial. Recognizing the symptoms of Alzheimer’s disease early allows for better planning, treatment options, and emotional preparedness for both patients and caregivers. The Alzheimer’s Association offers more information on how the disease develops.
Phases of Alzheimer’s Disease Progression
As the disease unfolds, it typically follows three main phases—each requiring different forms of care.
- Early Stage: Individuals may show mild forgetfulness and have trouble concentrating.
- Middle Stage: Behavior changes, confusion, and greater memory loss occur.
- Late Stage: Loss of ability to respond to the environment, speak, or control movement.
Tailored support is critical in each phase. Personalized care plans at Westmont of La Mesa are built to address these unique needs as Senior Alzheimer’s Disease progresses.
The Importance of Assisted Living Facilities
Choosing the right setting is key to managing Alzheimer’s disease treatment effectively. Assisted living communities like Westmont of La Mesa offer:
- Trained staff
- Safe, secure environments
- Daily routines for structure
- Cognitive and social activities
These communities provide comfort and dignity while alleviating the burden on families. Memory care outcomes also improve with active family involvement and thoughtful environments.

Personalized Activities for Engagement
Keeping seniors with Alzheimer’s Disease engaged is vital for slowing cognitive decline and improving emotional well-being.
Tailored Therapeutic Approaches
Activities such as art, gardening, and personalized music therapy are adapted to each resident’s abilities and interests. These programs help reduce anxiety and increase joy.
| Activity Type | Benefit |
| Music Therapy | Sparks memories and emotions |
| Art Therapy | Encourages self-expression |
| Light Exercise | Boosts mobility and energy |
Innovative Engagement Techniques
Memory care isn’t one-size-fits-all. Engagement in meaningful activities helps maintain purpose and connection, especially during the middle and late stages of Senior Alzheimer’s Disease.
These strategies—such as reminiscence therapy and sensory-based activities—are designed to match different types of Alzheimer’s disease and create uplifting moments for residents.
The Role of Family Support
Families play an irreplaceable role in Alzheimer’s care. Involvement in daily routines, emotional support, and attending care meetings can ease transitions and improve your loved one’s experience.
Communication and Connection
Navigating communication can be tough. As symptoms of Alzheimer’s disease worsen, patients may struggle to express their thoughts. Use simple sentences, validate feelings, and maintain eye contact. Activities like reviewing photo albums or listening to familiar music can bridge the gap.
Supporting the Caregiver
Caring for someone with senior Alzheimer’s disease can be emotionally draining. Families must also prioritize their own health. Support groups, counseling, and regular respite care can help prevent caregiver burnout.
Check out Family Caregiver Alliance for more caregiver-specific resources.
Emotional Challenges for Families
Coping With Grief and Loss
As the disease progresses, families often experience anticipatory grief—mourning the slow loss of the person they once knew. Journaling, meditation, and grief support groups can help.
| Strategy | How it Helps |
| Support Groups | Share experiences |
| Mindfulness Techniques | Reduce stress and anxiety |
| Counseling | Professional emotional support |
Exploring Types of Alzheimer’s Disease
There are several types of Alzheimer’s disease, and knowing the difference can guide care decisions:
- Early-Onset Alzheimer’s: Affects people younger than 65
- Late-Onset Alzheimer’s: Most common; occurs after 65
- Familial Alzheimer’s: A rare inherited form
Each type has a unique progression and may respond differently to Alzheimer’s disease treatment, making early diagnosis important.

Innovations in Alzheimer’s Disease Treatment
Medical and technological advances are changing the future of Alzheimer’s disease treatment:
- Medications like Donepezil and Memantine help manage symptoms
- AI-powered platforms assist in care planning and tracking behavior
- Telehealth and remote monitoring support more flexible care
Virtual reality and sensory stimulation are also emerging tools that engage the brain and spark joy in people living with senior Alzheimer’s Disease.
Learn more at NIH Alzheimer’s Research.
Planning for the Future
Proactive planning is one of the most loving things families can do:
- Schedule legal and financial planning early
- Choose a trusted healthcare proxy
- Tour memory care communities like Westmont of La Mesa
Starting the conversation early gives everyone more control and reduces stress later.
Ready to Take the Next Step? Let’s Talk.
Senior Alzheimer’s Disease affects millions, but you don’t have to navigate this journey alone. Whether you’re just noticing early symptoms of Alzheimer’s disease, exploring Alzheimer’s disease treatments, or searching for compassionate care tailored to different types of Alzheimer’s disease, help is available.
At Westmont of La Mesa, we provide expert memory care, personalized support, and a nurturing environment to ensure your loved one’s comfort and dignity every step of the way.
📞 Call us at 619-369-9700 or Schedule a Tour today.
Let’s make this journey a little easier—together.
Frequently Asked Questions
What is life like for a person with Alzheimer’s disease?
Life with Alzheimer’s disease often begins with mild memory lapses, such as forgetting names or misplacing items, and gradually progresses to more severe challenges. As the condition advances, daily routines may require assistance, and confusion about time or place can become common. Social interactions may feel overwhelming, leading some individuals to withdraw from activities they once enjoyed. However, with the right support, routines, and a compassionate environment, people with Alzheimer’s can still experience meaningful
What is the number one food to avoid dementia?
Research suggests that foods high in saturated fats and refined sugars, such as processed meats and fried foods, may increase the risk of dementia. These foods contribute to connections and moments of joy.
inflammation and poor cardiovascular health, both of which are linked to cognitive decline. Experts often recommend limiting processed foods and instead focusing on nutrient-rich diets like the Mediterranean diet. By emphasizing vegetables, fruits, whole grains, and healthy fats, individuals may better protect their brain health.
What are the behaviors of Alzheimer’s patients?
Alzheimer’s patients may display a range of behaviors, including confusion, agitation, or repetitive actions. Wandering is also common, as individuals may forget where they are going or why they left home. Mood changes, such as irritability, depression, or anxiety, can occur as the disease affects brain function. Caregivers often find that patience, redirection, and maintaining familiar routines help manage these behaviors.
What are the signs of Alzheimer’s in the elderly?
Early signs of Alzheimer’s in the elderly often include memory loss that disrupts daily life, like forgetting recent conversations or important dates. Difficulty solving problems, planning, or completing familiar tasks may also appear. Changes in mood, judgment, or withdrawal from social activities are other common symptoms. Recognizing these signs early is essential, as timely medical evaluation can lead to better management and care planning.